What to Expect…When Your Baby is Hungry
Lactation consultants offer vital support and coaching to parents and babies.

Courtney Walker-Borch and Gabrielle Bernier know better than most how eventful the first few days of parenthood can be.
“Few moments are as joyful — or as nerve-wracking — as holding your newborn baby and realizing you’re expected to know how to feed this tiny human,” says Walker-Borsch, MSN, APRN, an international board-certified lactation consultant (IBCLC) at University of Vermont Health - UVM Medical Center. “We’re here to help calm some of that anxiety and build healthy feeding habits from the get go.”
Walker-Borch and Bernier have nearly 25 years of combined experience as lactation consultants — part of the 15-strong team that provides around the-clock support for families at UVM Medical Center. They begin each day huddled in their office or with their colleagues at the nursing station. Together, they take stock of the families being cared for on the hospital’s mother-baby unit, assessing their feeding needs and overall health. Some are first-time parents; others are welcoming another child to their growing family. Regardless of their prior experiences, most encounter challenges feeding their newborn for the first time.
Teacher. Problem Solver. Emotional Support Person.
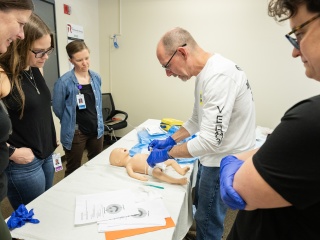
Enter lactation consultants — specialist caregivers who help parents learn to feed their babies, whether through breastfeeding, bottle feeding or a combination of the two. It’s a mix of teacher, problem-solver, coach and emotional support specialist.
“You’re tired…your baby is hungry and having trouble latching — it can be a lot,” says Gabrielle Bernier, IBCLC, who has been a lactation consultant at UVM Medical Center for the past three years. “All of these things are so normal, and often times people just need a little reassurance and the right tools to help them find their healthy feeding rhythm.”

No Pressure. Just Support.

On a typical day, Bernier and Walker-Borch work hands-on with parents and babies, helping them with things like positioning and latch (how the baby attaches to the breast), assessing milk supply, managing pain or nipple injury and troubleshooting common issues such as engorgement, clogged ducts or mastitis. As part of their routine, they evaluate how well a baby is feeding — watching a full feeding, checking weight gain patterns and helping adjust technique so the baby gets the nutrients they need.
They also teach parents how to use breast pumps, store milk safely, maintain supply when returning to work, and make feeding plans that fit real life — not some idealized version of it.
“We’re not here to pressure anyone to feed their baby in particular way,” says Walker-Borch. We’re here to make sure families feel informed, confident and supported during a really vulnerable period of early parenthood.”
Beyond the Mother-Baby Unit
It’s not just fledgling families in the mother-baby unit that need lactation support. Staff and patients elsewhere in the hospital often turn to the lactation consultant team to troubleshoot feeding difficulties.
“People come to the hospital for so many reasons, and some are still in the early stages of learning to feed their newborn,” says Walker-Borch. “We may not be in a position to help treat that person, but we can certainly help care for them and their baby by working on their feeding goals while they’re here.”